A CASE OF 26 YEAR OLD MALE WITH SOB, COUGH AND FEVER
A 26 year old male presented with c/o SOB, cough and fever since 2 days.
History of presenting illness:
Patient was apparently asymptomatic 2 days back then he developed SOB initially grade 2 now progressed to grade 4 associated with cough, non productive, noy associated with blood.
C/o fever since 2 days.
He had similar complains 4 months back for which he was admitted.
His earliest recall of events dates back to when he was studying in high school ( 9th class ) during the lunch break, he felt severe breathlessness and had to sit back while playing with copious amounts of ?sputum expectoration which he describes it as yellowish in colour and non foul smelling, he describes the incident like he is an old man and needs to sit back to catch up breath.
He continues to feel breathlessness through out his teens and he needs to rest often associated with palpitations on further asking to describe the palpitations it was of pounding nature ( in his words hitting a wall with loud thump ) lasting for 1-2 hours aggravating on lying down
He often developed respiratory tract infections with history cough with copious amounts of expectorant, sore throat and running nose with is relieving on taking medication ( tab azithromycin).
On asking his mother she gave a long history of repetitive infections since childhood once or twice a year and avoiding foods aggravating his cough and cold he was taken to hospital at one year of age for breathlessness.
He’ss the third born child with term pregnancy normal vaginal delivery with meconium aspiration and was diagnosed to be dextrocardia on 4th day of delivery as he was sick they were referred to many hospitals and was discharged after relieving his symptoms.
He was also advised to practice to sit with head low and knees apposed to chest which resulted in vain
He’s married to his wife and alcohol since two years with occasional binge ( once or twice weekly ) whiskey preferably (90-180ml ) says post binging breathlessness decreases and doesn’t get sputum,he works as an VRO ( village revenue officer ) since after his father was retired and finds it difficult as its not a desk job and halts regularly to catch up breath.
14 days back under the influence of alcohol he had a history of fall from bike
Sustained head injury with no history of loss of consciousness, ENT bleed and denied going to hospital as he was alright and developed fever on subsequent day subsided on medication
History of pedal oedema since 10 days extending upto knee pitting type progressively increasing and attained the present state, he denies history of pedal oedema prior to these 10 days and also denies history of hematuria and frothy urine or decreased urine output and facial puffiness
3 days back on occasion of raksha bandhan
Post binge he had 3 episodes of vomiting in the morning was taken to a local doctor revealing potassium 3.2 and creatinine 2.2,TLC -16000 and was given fluids and antiemetic medication
Since 3 hours he developed breathlessness post binge and was brought to casualty with spo2 41% on RA and 84% on 15L of oxygen
General examination:
Patient is conscious and cooperative
No pallor, icterus,
cyanosis
With clubbing of fingers and pedal edema.
No generalised lymphadenopathy.
Vitals:
Temperature - 97.6
Pulse- 104 bpm
RR- 38 cpm
BP- 90/60 mmHG
SPO2- 60% at RA.
CVS: S1 and S2
RS: B/L crepts IAA and
IMA
P/A: Soft and non tender
Provisional diagnosis:
Kartageners syndrome with viral pneumonia
Investigations:
ABG:
PH: 7.35
PO2 : 79.9
PCO2: 53.5
HCO3-: 29.3
St. HCO3-: 26.6
LFT:
Tb: 2.62
Db: 0.62
Ast: 25
Alt: 22
Alp: 170
Alb: 2.2
RFT:
Urea: 37
Creatinine: 1.1
UA: 8.6
Ca2+: 10.2
PO4-3: 4.2
Na+ : 140
K+: 5.5
Cl- : 92
Hemogram
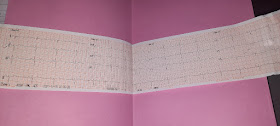
Ecg on 18/12/21:
At 1 am
At 3 am
At 7 am
PROVISIONAL DIAGNOSIS :
CHRONIC COR PULMONALE SECONDARY TO BRONCHIECTASIS,VIRAL PNEUMONIA
K/C/O KARTAGENERS SYNDROME ( SITUS INVERSUS)
C/O SOB Grade 4 ( not subsiding)
TREATMENT :
1. Neb BUDECORT 12th hourly
IPRAVENT 8th hourly
2. Inj. LASIX 2O MG IV BD ONLY IF SBP >110 MMHG
3. Inj. PAN 40MG IV OD
4. Inj. DOBUTAMINE 1 AMP in 48 mins at 5 ml /hr
5. Tab. PCM 650 MG PO SOS
6. Intermittent CPAP
7. Inj. NA at 6ml/hr
8. Inj. AUGMENTIN 1.2 gm/ IV BD
9. Tab. AZITHROMYCIN 500MG OD
10. monitoring vitals
On 19/12/2021
PROVISIONAL DIAGNOSIS :
CHRONIC COR PULMONALE SECONDARY TO BRONCHIECTASIS,VIRAL PNEUMONIA
K/C/O KARTAGENERS SYNDROME ( SITUS INVERSUS)
C/O SOB Grade 4 ( not subsiding)
TREATMENT
1. Neb BUDECORT 12th hourly
IPRAVENT 8th hourly
2. Inj. LASIX 2O MG IV BD ONLY IF SBP >110 MMHG
3. Inj. PAN 40MG IV OD
4. Inj. DOBUTAMINE 1 AMP in 48 mins at 5 ml /hr
5. Tab. PCM 650 MG PO SOS
6. Intermittent CPAP
7. Inj. NA at 6ml/hr
8. Inj. AUGMENTIN 1.2 gm/ IV BD
9. Tab. AZITHROMYCIN 500MG OD
10. monitoring vitals










Comments
Post a Comment